Med-surg Hesi Study Guide 5c5dr
This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 2z6p3t
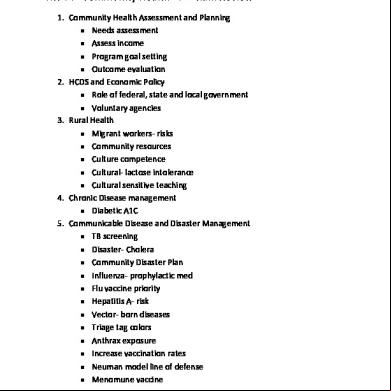
Overview 5o1f4z
& View Med-surg Hesi Study Guide as PDF for free.
More details 6z3438
- Words: 4,390
- Pages: 21
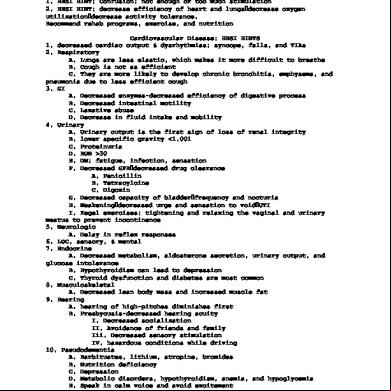
Geriatrics 1. HESI HINT: Confusion: not enough or too much stimulation 2. HESI HINT: decrease efficiency of heart and lungs×decrease oxygen utilization×decrease activity tolerance. Recommend rehab programs, exercise, and nutrition Cardiovascular Disease: HESI HINTS 1. decreased cardiac output & dysrhythmias: syncope, falls, and TIAs 2. Respiratory A. Lungs are less elastic, which makes it more difficult to breathe B. Cough is not as efficient C. They are more likely to develop chronic bronchitis, emphysema, and pneumonia due to less efficient cough 3. GI A. Decreased enzymes-decreased efficiency of digestive process B. Decreased intestinal motility C. Laxative abuse D. Decrease in fluid intake and mobility 4. Urinary A. Urinary output is the first sign of loss of renal integrity B. lower specific gravity <1.001 C. Proteinuria D. BUN >30 E. DM: fatigue, infection, sensation F. Decreased GFR×decreased drug clearance A. Penicillin B. Tetracylcine C. Digoxin G. Decreased capacity of bladder×frequency and nocturia H. Weakening×decreased urge and sensation to void×UTI I. Kegel exercises: tightening and relaxing the vaginal and urinary meatus to prevent incontinence 5. Neurologic A. Delay in reflex responses 6. LOC, sensory, & mental 7. Endocrine A. Decreased metabolism, aldosterone secretion, urinary output, and glucose intolerance B. Hypothyroidism can lead to depression C. Thyroid dysfunction and diabetes are most common 8. Musculoskeletal A. Decreased lean body mass and increased muscle fat 9. Hearing A. hearing of high-pitches diminishes first B. Presbycusis-decreased hearing acuity I. Decreased socialization II. Avoidance of friends and family Iii. Decreased sensory stimulation IV. hazardous conditions while driving 10. Pseudodementia A. Barbituates, lithium, atropine, bromides B. Nutrition deficiency C. Depression D. Metabolic disorders, hypothyroidism, anemia, and hypoglycemia E. Speak in calm voice and avoid excitement
c c c
Respiratory 1. Pneumonia A. Increased respiratory rate B. Irritability and restlessness C. Fever, shaking, crackles (lungs are filled with fluid) D. Chills, productive cough (alveoli is filled with fluid) E. Confusion and lethargy in elderly F. Assess ABGs G. Deep breath, cough, suction H. Hint: irritability and restlessness are the first signs of cerebral hypoxia I. provide hydration J. Difficulty breathing×stiff lungs×hypoxia K. Decreased breath sounds×congested lungs 2. Always give steroids last A. Follow with oral hygiene due to risk of super-infection 3. Singulair (a leukotriene) A. chronic asthma 4. oral suctioning is not sterile 5. Mask, gloves, and goggles for suctioning 6. Acute Respiratory Failure A. Ph less than 7.35 B. Oxygen less than 50 C. C02 greater than 50
Neurosensory 1.
2. 3. 4. 5. 6. 7.
8.
c c c
Encephalitis A. Vitals I. Widened pulse pressure II. Bradycardia III. Irregular respirations IV. Eyes do not PERRLA V. Elevate head of the bed to 30 or 45 degrees Parkinson¶s A. Dopamine Hydrocephalus A. II B. 6th nerve defect Meningitis A. 3, 4, 6, 7, 8 Lumber puncture A. Measure pressure in CSF B. Indicate neuro disorders, infections, brain, or spinal cord damage EEG A. Avoid caffeine and hair products before the test II A. Compresses brain structures B. Reduces blood flow C. Widened pulse pressure D. Bradycardia E. Increased temp. F. Cheyne-stokes G. ister oxygen and monitor intake and output H. Elevate head of bed 30-45 degrees Seizures A. Prodromal
I. Mood changes, irritability, insomnia 9. Meniere¶s Disease A. Salt-free diet B. Vasodilators C. Neuroleptics D. Diuretics E. Anti-histamines F. Anti-cholingergics G. Sedatives H. Encourage slow movement 10. Acute closed angle glaucoma A. Severe eye pain B. halos C. Pupils dilate D. nausea and vomiting E. ister stool softeners, constrictive clothing, and colds 11. Detached retina A. Sclera buckling
Cardiovascular 1. Peripheral Vascular Disease A. Arterial I. Arteriosclerosis & Atherosclerosis II. Raynaud, Buerger, and Diabetes diseases III. Smooth, shiny skin with loss of hair IV. Thickened nails V. pale when elevated, rubor when dependent VI. Decreased or absent pulses (impaired perfusion) VII. Sharp pain; intermittent claudicateion VIII. necrotic ulcers on lateral lower legs, toes, and heels IX. cool temperature (reduced blood supply) X. pain is relieved when dependent XI. numbness and tingling (impaired perfusion) Ai I. Anti-platelets to thin blood) ii. anti-hypertensives iii. anti-coagulants iv. exercise B. Venous I. DVT and valvular disorders II. Varicose veins III. venous stasis ulcers iv. brown pigment around ankles v. cyanotic when dependent vi. normal pulses vii. ulcers on medial legs and ankles viii. marked edema ix. elevate extremities for relief x. warm temperature C. Avoid crossing legs and wearing constrictive clothing D. Keep legs dependent if arterial, and elevated if venous E. Compression dressing for venous 2. AAA A. abdominal and back pain (pressure on lumbar nerves) B. Bruit
c c c
C. Asses peripheral pulses (tachycardia and hypotension indicates hemorrhage or shock) D. Neuro (brain is not being perfused) E. Vitals I. Impending shock and graft occlusion F. Renal i. artery clamped×kidney damage ii. BUN and creatnine G. graft occlusion I. change in pulses ii. pain iii. coolness below graft iv. white or blue extremities H. pulsatile mass I. 3. DVT A. calf pain B. edema C. warmth and redness D. tender areas E. Notify doctor of abnormal bleeding during drug therapy F. avoid aspirin G. wear anti-embolism stockings H. anti-coagulants I. elevate leg 4. Valvular disorders A. Decreased cardiac output B. impaired gas exchange C. stenosis or regurgitation D. mitral valve most commonly effected *E. prophylactic treatment before dental work to prevent infection of the heart, and lifelong anticoagulant therapy F. 5. Endocarditis A. vegetation adhere to the valve surface of endocardium B. Fever, chills, malaise, fatigue, splenomegaly, C. Murmur *D. Symptoms of heart failure E. *treat with antibiotics 6. Pericarditis A. friction rub B. substernal pain radiating to back and arm, worst on inspiration, better when leaning forward C. Fever D. Dysphagia (fluid around heart places pressure on esophagus) E. Tachypnea 7. Cardiac tamponade A. JVD (heart is squeezed, so blood backs into circulation) B. hypotension (decreased cardiac output) C. muffled heart sounds (due to fluid accumulation) D. pulsusparadoxius (pulse drops during inspiration) E. decreased LOC F. Increased HR G. edema H. *treat with 02 8. Atherosclerosis
c c c
A. life-style modification B. nitrates C. antihypertensive d. anti-coagulants e. calcium-channel blockers f. ACE inhibitors g. anti-platlets µ 9. Arteriolosclerosis A. arteries harden and thicken B. vitals organs are not adequately perfused C. kidneys are most affected 10. Buerger¶s disease A. inflammation and blockage of small and medium sized arteries of the extremities B. Caused by smoking (causes inflammation and constriction of blood vessels) C. claudication D. numbness and tingling E. skin ulcerations and gangrene 11. How to calculate mean arterial pressure A. (SBP+2DP)/3 i. less than 60 indicates inadequate perfusion 12. PTT a. 16-40 normally 13. Central venous pressure A. 5-10 cm water 14. Stenosis-blood flow is impeded 15. regurgitation-backward leakage of blood 16. Mitral valve disorders (both sided heart failure) 17. Aortic disorders-left side heart failure 18. Avoid green leafy vegetables while taking warfarin 19. APPT with heparin: 60-80 seconds
Gastrointestinal System 1. Hiatal Hernia A. Portion of the stomach protrudes through esophageal hiatus B. Feeling of fullness C. Feeling of suffocation and smoothing after meals (eating distends the stomach, leading to decreased ability of the lungs to expand D. Breathing difficulty E. Anemia F. *sit up after eating 2. GERD A. Pain, burning, and dysphagia (scarring from irritation) B. Eat low fat, high protein foods C. Limit chocolate and mints D. Avoid carbonated beverages E. Proton pump inhibitors (zole) F. H2 receptor blockes (dine) G. Antacids H. mucosal barrier fortifiers (sucralfate-Carafate) I. Can lead to stricture and barret¶s esophagus 3. Peptic ulcer disease
c c c
A. Erosion of the lining of the stomach, pylorus, duodenum, or esophagus due to exposure of hydrocholoric acid, pepsin, and H. pylori infection B. Caused by NSAIDS, alcohol, smoking, anti-coagulants, and trauma C. Belching, bloating, epigastric pain, indigestion, pain after eating, nausea, and vomiting D. Gastric: eating causes pain; Duodenal: eating helps pain Treatments: A. avoid spicy foods B. Give cytotec and other anti-ulcer meds C. Antacids neutralize gastric acid D. Monitor for i. dark, tarry stools (melena) ii. coffee-ground vomit iii. bright red rectal bleeding iv. fatigue v. pallor vi. abdominal pain vii. abdominal mass or bruit viii. decreased BP, rapid pulse, cool extremities Treatments A. saline lavage B. NPO and IV fluids 4. Perforation A. ulcers penetrating the wall of the GI tract B. sudden, excruciating pain in shoulders C. becomes more intense with position change and deep breathing D. Rebound tenderness E. fever Treatments A. ister fluids B. NG suction C. emergency surgery 5. Stomatitis A. ask about nutrition, oral hygiene, antibiotic use, use of mouthwash and toothpaste B. Use soft bristle tooth brushes C. Avoid spicy foods D. Viscous lidocane-can numb throat and impair swallowing E. *risk for impaired nutrition and fluid volume deficit 6. Gastritis (inflammation of stomach lining) A. Pain, heartburn, belching, bloating, loss of appetite, and weight loss, bleeding B. Antacids and anti-biotics due to H. Pylori infection 7. Gastroenteritis A. inflammation of GI tract B. *Diarrhea (large intestine cannot retain fluids): hallmark sign C. abdominal cramps due to inflammation D. loss of appetite E. dehydration due to diarrhea F. weakness and fatigue due to nausea and vomiting G. obtain history of travel and recent foods eaten Treatments A. replacing fluids and electrolytes B. avoid dairy products, vegetables, and fruits
c c c
C. avoid caffeine D. perform skin care due to diarrhea E. avoid raw meat, fruit, and vegetables during travel F. Do not use tap water or ice G. monitor for s/sx of dehydration: decreased urination, dry skin and mucous membranes, dark urine, decreased BP, low potassium and sodium levels, and elevated BUN 8. Malabsorption A. nutrients are digested or absorbed properly B. Weight loss C. steatorrhea due to decreased fat absorption D. diarrhea E. increased bruising F. edema due to decrease protein absorption G. anemia due to vitamin B12, and iron deficiency 9. Polyps A. Bleeding due to polyp irritation B. Abdominal pain and cramping due to obstruction of GI contents C. Diarrhea due to polyp excretion of water and salts Treatments A. polypectomy B. increase calcium intake C. exercise D. low fat, high fiber diet 10. Hemorrhoids A. bleeding due to irritation B. itching due to inadequate cleaning of rectum C. pain Treatments A. sitz bath B. creams and ointments C. compress pads and wiping with moist wipes D. high fiber diet and increase fluids E. stool softener F. avoid long periods of sitting 11. Dumping syndrome A. sweating B. fatigue and desire to lie down C. palpitations D. light-headedness and syncope E. flushing F. abdominal pain and cramping G. hunger Treatments A. restrict fluid during eating B. eat small frequent meals C. lie flat on left side after eating D. decrease carbs and increase fat and proteins E. dietary fiber supplements F. anti-cholinergics 12. Hernia A. Inguninal, femoral, umbilical, and incisional B. caused by increased abdominal pressure and abdominal surgery C. new onset pain and tenderness indicate strangulation D. Decrease abdominal pressure E.provide stool softeners
c c c
F. Avoid coughing post op and increase fluids 13. Intestinal obstruction A. abdominal cramping and pain due to obstruction B. distention because foods or gas cannot the obstruction C. bowel changes D. decreased bowel sounds distal to obstruction E. vomiting due to accumulation of fluids F. fluid and electrolyte imbalances due to inability to absorb nutrients G. Fever due to infection Treatments A. NPO B. NG tube low to suction to remove contents C. Fluid and electrolyte replacement D. withhold pain meds 14. Appendicitis A. pain around umbilical area B. fetal position helps relieve pain C. abdominal guarding D. pain increases with cough and movement and relieved by flexion of knees (rupture) E. nausea and vomiting F. AVOID USING HEAT! G. DO NOT GIVE LAXATIVES OR ENEMAS H. NPO I. IV fluids J. antibiotics 15. Peritonitis (risk for shock) A. inflammation of peritoneum B. pain C. rebound tenderness D. abdominal rigidity E. board like abdomen (widespread inflammation) F. decreased bowel sounds G. increased pulse (hypovolemia) H. decreased urinary output (decreased fluid in circulation) I. nausea and vomiting J. fluid and electrolyte imbalances Treatments A. NPO B. IV fluids and electrolytes C. antibiotics D. NG insertion E. peritoneal lavage to indicate GI bleeding F. oxygen and semi-fowler¶s position *can lead to septicemia, shock, and respiratory distress 16. Crohn¶s disease A. portion of small intestine thickens and narrow the lumen B. Pain, vomiting and diarrhea C. weight loss and malabsorption D. elevate temperature E. fluid and electrolyte imbalances due to malabsorption F. NPO for bowel rest G. low residue diet: low fiber, low fat diet high in calories, carbs, proteins, and vitamins
c c c
H. I. J. K.
corticosteroids anti-diarrheals antibiotics Increase calories and fluids to heal fistulas
17. Ulcerative colitis A. inflammation of large intestine and rectum B. 10-20 liquid stools per day C. rectal bleeding D. increased bowel sounds E. weight loss F. *bloody diarrhea mixed with mucous G. anemia H. NPO I. TPN J. low-residue foods, low-fat, high protein, high calories food K. Avoid milk and encourage bed rest L. anti-diarrheals M. sulasalazine 18. Irritable bowel syndrome A. altered intestinal motility B. diarrhea, constipation, or both C. bloating and gas D. Increase fiber and give laxatives for constipation E. anti-diarrheals and increase fluids for diarrhea F. avoid caffeine, dairy foods, and fructose G. bulk-forming laxatives for constipation H. anti-depressants I. Imodium for diarrhea 19. Diverticulitis A. inflammation or infection of blind pouches B. pain C. fever D. weakness E. diarrhea F. anemia caused by rectal bleeding G. do not do barium enema or colonoscopy during diverticulitis H. liquid diet initially I. low fiber diet J. avoid laxatives K. *signs of intestinal obstruction L. acute phase: NPO or liquids M. recovery: no fiber or foods N. maintenance: high fiber with bulk forming laxatives. Avoid popcorn, nuts, or seeds 20. Ileostomy drains liquid, increasing risk of skin breakdown 21. Pouch system is changed every 3-7 days 22. Cirrhosis A. fatal scarring and fibrosis of liver tissue B. Jaundice due to bilirubin build up C. Pruritis& clay colored stools D. ascites due to decreased albumin (albumin keeps fluid in vascular space) E. hepatomegaly F. nausea due to toxin buildup
c c c
G. spider angiomas (decreased vitamin K) H. increased medication sensitivity I. splenomegaly (decreased platelets and WBCs) J. Esophageal varices (portal hypertension) K. Neuro deficits (increased ammonia buildup): encephalopathy L. shortness of breath M. increased bilirubin, albumin, ALT & AST, PT, serum ammonia Treatments A. take vitaminas B. sodium and fluid restriction C. frequent rest periods D. diuretics E. albumin istration F. elevate head 30 degrees G. monitor meds H. monitor esophageal bleeding 23. Cholecystitis A. inflammation of gallbladder B. pain righting to right shoulder and scapula C. nausea and vomiting due to pain D. fever, elevated liver enzymes, and bilirbun E. steatorrhea&jaunide f. NPO initially G. low fat diet H. anti-spasmodics and anticholinergics I. morphine can cause spasms J. IV hydration and pain control K. decompress stomach with NG tube 24. Pancratitis A. enzymes are activated while still in pancreas B. autodigestion C. Pain radiating to back or epigastrium radiating to left should or back D. decreased bowel sounds E. respiratory distress caused by enzymes entering pleura cavity F. cullen¶s sign (blue color around umbilicus) G. decreased LOC h. turner¶s sign (gray color of flank) I. ascites J. steatorrhea Treatments A. IV fluids and electrolytes B. NPO C. prophylactic antibiotic D. oxygen istration E. NG low to suction F. pain management G. replacement of pancreatic enzymes H. insulin I. measure abdominal girth
OTHER GI NOTES 1. The barium swallow study detect anatomic and functional changes of the esophagus, stomach, and small intestine. A. laxatives and fluids are given after the test 2. The barium enema study detects changes of the large intestine.
c c c
3. Clear liquid diet indicated for endoscopic studies. 4. Monitor cardiac and respiratory functions after EGD procedure 5. Antacids and H2 receptor antagonists should not be given before gastric analysis. A. Pernicous anemia B. Zollinger-Ellison¶s syndrome 6. Place on right side after liver biopsy 7. TPN for GI motility disorders and dysfunction A. check weight and glucose levels B. monitor for infection and air embolism 8. GERD: avoid citrus fruits, caffeine, garlic, fried foods, onions, and tomato-based products 9. Gastric resection (Bilroth I & II): NPO until suture line heals 10. Dumping syndrome: avoid high-carb meals; eat high-protein, high-fat, low carb meals 11. IBS: pain relieved by sleeping and having a bowel movement 12.
13. Hepatitis: focus on prevention
c c c
14. Cirrhosis: normal liver cells are replaced with scar tissue 15. Regular functions of the liver: A. synthesis of clotting factors B. metabolism of hormones (aldosterone, ADH, estrogen and testerone) C. synthesize albumin (maintains normal colloid pressure) D. carb, protein, and fat metabolism E. filtration of drugs F. storage of vitamins and minerals 16. Early stages of cirrhosis: enlarged liver, jaundice, GI disturbances, abdominal discomfort 16.late stages: enlarged spleen, ascites, bleeding tendencies, esophageal varices, dyspnea, pruritis, clay-colored stools 17. end-stage: heptatis encephalopathy 18. Encourage rest, decreased fluid intake, high-calorie, low-protein, lowsodium, low-fat diet, assess abdominal girth, diuretics, lactulose, IV fat soluble vitamins and albumin
c c c
A. low-protein due to the body¶s inability to secrete ammonia, lowsodium to prevent ascites, low-fat diet due to the liver¶s inability to break down fats 19. Varices in the esophagus bleed due to coughing, trauma, and vomiting 20. Murphy sign A. extreme pain on deep inspiration: cholecystitis 21. Greatest risks for pancreatitis are those suffering from alcohol abuse, liver, and gallbladder disease 22. Do not give ice chips and hard candies to prevent stimulation of pancreas 23. Major complication of liver biopsy is hemorrhage, so assess PT prior to procedure 24. GGT assesses possibility of alcohol abuse 25. Fatty foods have no direct effect on diverticulitis 26. Ginger root has antiemetic, analgesic, and sedative properties 27. Bariatric surgery results in the construction of a small pouch in the upper part of the GI. Overfilling of the pouch leads to nausea 28. *Zenker¶s diverticulum is an outpouching of the esophagus near the hypopharyngealspincter. Risk for aspiration 29. Weight can cause a non-alcoholic fatty liver 30. Beta-blockers are given in cirrhosis to prevent esophageal varrices bleeding 31. Positioning the client on the right side after a liver biopsy splints the puncture site to prevent and decrease bleeding. 32. Grey-Turner sign in pancreatitis-blood-stained exudates from the pancreas indicates a severe disease process 33. Patients with IBS have mucous in stools 34. Bowel strictures in Crohn¶s disease can lead to obstruction 35. Patients are placed in side-lying position after anorectal surgery 36. Asprin decreases risk of colon cancer 37. Peristalsis do not return for 3-5 days after abdominal surgery
c c c
DIABETES 1. Type I A. Glucose usually 350 and above B. Ketonuria C. Bicarbonate less than 15 D. Clients are usually thin and under 30 2. Type II. A. *nonketotic hyperosmolar hyperglycemia B. Plasma hyperosmolality C. Dehydration D. change in mental status 3. Assessment: A. Breaks in skin B. Dental caries and fungal infection C. Cataracts and diabetic retinopathy D. Chest pain and shortness of breath E. Hair loss on extremities with non-palpable pulse, pallor, and ulcerations F. Edema of face, hands, feet, and urinary retention G. Neuropathies H. night time diarrhea I. vaginal dryness and frequent yeast infections 4. Take meds according to insulin peak times 5. Eat bedtime snacks 6. Wash feet daily but DO NOT soak! Dry them well 7. Do not moisturize feet between toes 8. Sandles should be avoided 9. Do not wear garters or elastic topped socks 10. Stress and illness can cause hyperglycemia 11. Hypovolemia (polyuria)
Oral meds 1. Sulfonylureas (Glyburide &glipizide) A. stimulates the release of insulin from pancreas and tissues take up glucose more easily B. hypoglycemia is adverse reaction C. Give with meal once daily 2. Biguinides (metformin) A. inhibit hepatic glucose production and increase sensitivity of tissue to insulin B. GI disturbances 3. Thiazolidinediones (actos&avandia) A. decrease insulin resistance to the tissues B. weight gain and edema 4. Alpha-glucosidase inhibitors A. decrease blood glucose absorption B. take with first bite of each meal 5. Meglitindes A. same as sulfonylureas
c c c
*Insulins 1. Rapid acting A. Humalog &Novolog B. 5-15 minutes onset C. 45-1.5 hours peak D. Give within 5-15 minutes of meal 2. Short acting A. Regular insulin B. 30-60 minutes onset C. 2-3 hours peak 3. Intermediate A. NPH &Humulin L B. 1-2 hours onset C. 6-12 hours peak 4. Long acting A. Lantus B. 4-8 hours onset C. 14-20 hours peak D. Give at bedtime E. Bottle is shaped differently than regular insulin, but is clear F. Do not shake or mix with other insulins
1. 2. 3. 4. 5. 6.
Diabetic ketoacidosis Body breaks down fat-×ketones Metabolic acidosis decreased LOC hypovolemia (excess sugar and fluid is excreted) electrolyte imbalances (hyperkalemia) Kussmaul respirations to blow off excess acid
*monitor for hyperglycemia hyperosmolar nonketotic syndrome 1. Extremely high glucose 2. elevated BUN Hypoglycemia 1. soda, orange juice, apple juice, or hard candy 2. complex carbohydrate (half of peanut butter sandwich, milk, and cheese crackers
c c c
Other notes 1. post-pandrial glucose is less than 140 2. A1C: 4-7% 3. Diabetics have increased risk for infection 4. Cool, clammy skin is often seen in hypoglycemia 5. in diabetic ketoacidosis, the skin is flushed due to dehydration and poor skin turgor A. ister IV saline, potassium and insulin 6. A bedtime snack is not needed with long-acting insulin 7. Exercising with glucose levels exceeding 250 and ketonuria increases secretion of glucagon, growth hormone, and catecholamines, casuing the liver to release more glucose
Fluids Imbalances 1. Organs involved: A. kidney (fluid and electrolyte, acid-base balances) B. lungs (acid-base balance, rid 300 ml of fluid) C. heart (kidney perfusion) D. adrenal gland (secrete aldosterone) E. pituitary gland (secrete ADH) F. parathyroid gland 2. Fluid volume deficit: A. loss of water, electrolytes remain normal, but sodium increases) B. Decreased skin turgor C. oliguria D, dry and sticky mucous membranes E. weak, rapid pulse F. Elevated BUN (measures excretory function of kidney) G. elevated Creatnine H. Increased serum osmolarity (amount of solvent is decreased) I. Elevated Hgb and Hct J. Replace isotonic fluids because water is hypotonic K. Strict I & o L. Increased urine osmolality (due to concentrated urine) i. 1.001-1.030 3. Fluid volume excess: A. Body retains water, sodium level decreases B. Heart, renal, liver failure C. Peripheral edema D. bounding pulse with increased BP E. distended neck and hand veins F. dyspnea G. All lab values decreased (hemodilutional state with diluted urine) H. Diuretics I. Fluid and salt restriction J.Strict I & O K. Weigh daily
c c c
Electrolyte Imbalances 1.c Sodium: 135-145 2.c Potassium: 3.5-5 3.c Calcium: 9-10.5 4.c Magnesium: 1.3-2.1 5.c Chloride: 95-105 6.c Phosphate: 3-4.5 Abnormalities and common causes Hyponatremia -diuretics -hypotonic solutions -sweating
Hypernatremia -water deprivation -watery diarrhea -renal failure
Hypokalemia -diuretics -vomiting -NG suctioning
Hyperkalemia -oliguria -renal failure -acidosis
Hypocalcemia -renal failure -hypoparathyrodism -malabsorption
Hypercalcemia
c c c
S/Sx
Treatment
- muscle weakness (decreased excitability of cell membranes) -seizures -muscle cramps -twitching -lethargy and confusion Thirst -tachycardia (heart is trying to pump around what little fluid is left) -dry mouth -irritability -muscle weakness (potassium is needed for muscle contraction) -decreased GI motility -dysrhythmias -paresthesia -slow, difficult respirations (respiratory muscles are weak) -bradycardia -dysrhythmias -flaccid paralysis (excessive potassium interferes with muscle contraction) -diarrhea -numbness and cramps -tingling of extremities -convulsions (muscles contract) -positive trousseau sign (hyperexcitability of hand muscles) -positive chvostek¶s sign (hyperexcitabilty of facial muscles) -laryngeal spasms -increased DTRs -constipation
-restrict fluids -hypotonic or hypertonic saline solutions -increase dietary sodium
-restrict sodium -increase water intake
-never give bolus (do not exceed 20 meq) -assess renal status before istration -eat bananas, oranges, cantaloupes, avocados, spinach, potatoes -ister potassium chloride ister 50% glucose with regular insulin -ister kayexalate -ister calcium gluconate -IV loop diuretics -ister calcium IV slowly -vitamin D
-ister
-hyperparathyroidism
-polyuria -polydipsia -dysrhythmmias -respiratory arrest (sedative respiratory muscles) -decreased bowel sounds (intestines are sedated) -muscle weakness (sedated muscles)
calcitonin(moves calcium into the bones) -IV phosphate
Hypomagnesemia -alcoholism -diabetic ketoacidosis -malabsorption
same signs and symptoms of hypercalcemia -BP increases (vasoconstriction)
-ister magnesium sulfate
Hypermagnesemia -renal failure
-flushing -hypotension -drowsiness -depressed respirations -hypoactive reflexes -bradycardia -BP decreases (vasodilation) -facial flushing and warming (vasodilation) -sedated respiratory muscles -parestheias -muscle weakness -cardiomyopathy -respiratory failure -(SIGNS AND SYMPTOMS OF HYPERCALCEMIA) -tentanysymptons (SIGNS AND SYMPTOMS OF HYPOCALCEMIA)
Avoid magnesium based antacids and laxatives -0.45 saline solution -IV calcium gluconate -loop diuretics -respiratory
Hypophosphaemia -alcohol withdrawal
Hyperphosphatemia -renal failure
-IV phosphorus when serum level drops below 1
ister aluminum hydroxide -ister vitamin D
Other notes 1. hyponatremia caused by hypervolemia: fluid restriction
c c c
Acid-base balance 1. 20 bicarbonate to 1 carbonic acid ratio 2. Respiratory acidosis A. Pulmonary disease B. Sleep apnea 3. Respiratory alkalosis A. over-ventilation B. response to hypoxia C. fever 4. Metabolic acidosis A. lactic acidosis B. ketoacidosis C. acid ingestion 5. Metabolic alkalosis A. Gastric drainage B. vomiting C. burns
Peri-operative 1. Surgical risks A. young and old B. obese and malnourished C. dehydrated D. clients with any infection E. cardiac conditions F. blood coagulation disorders G. upper respiratory tract infections and COPD H. renal disease (renal insufficiency) I. diabetes due to delayed healing and possibility of wound infection J. Use of anticoagulants K. use of antibiotics (may be incompatible to anesthesia) L. diuretic use (electrolyte imbalances) M. steroids N. vitamin E use 2. Client has to be 18 to sign surgical consent form c Pre-operative 1. Client teaching: A. Coughing and deep breathing B. ing the wound by splinting C. leg exercises D. Turning, positioning, ambulation E. Recovery room procedures F. Type of dressing, NG tubes, drains, foley catheter G. Decreases anxiety and promotes client participation H. Regulations about jewelry I. NPO status J. Dietary restrictions K. informed consent must be signed before the istration of medications
c c c
Intra-operative 1. report changes in pulse, temperature, respirations, and blood pressure to surgeon . Postoperative 1. Signs A. B. C. D.
of shock and hemorrhage hypotension tachycardia narrowed pulse pressure cold, moist skin
2. Post-op care A. Pulmonary i. Airway (check gag reflex) ii. Bilateral breath sounds iii. Deep breathing and coughing B. Neuro i. LOC ii. Reflexes C. Circulation i. Vital signs ii. Peripheral perfusion D. GI i. Bowel sounds ii. Distention E. GU i. Urinary output ii. Intake and output *malignant hyperthermia *somogyi/dawn effect *smoking-pack years
c c c
c c c
c c c
Respiratory 1. Pneumonia A. Increased respiratory rate B. Irritability and restlessness C. Fever, shaking, crackles (lungs are filled with fluid) D. Chills, productive cough (alveoli is filled with fluid) E. Confusion and lethargy in elderly F. Assess ABGs G. Deep breath, cough, suction H. Hint: irritability and restlessness are the first signs of cerebral hypoxia I. provide hydration J. Difficulty breathing×stiff lungs×hypoxia K. Decreased breath sounds×congested lungs 2. Always give steroids last A. Follow with oral hygiene due to risk of super-infection 3. Singulair (a leukotriene) A. chronic asthma 4. oral suctioning is not sterile 5. Mask, gloves, and goggles for suctioning 6. Acute Respiratory Failure A. Ph less than 7.35 B. Oxygen less than 50 C. C02 greater than 50
Neurosensory 1.
2. 3. 4. 5. 6. 7.
8.
c c c
Encephalitis A. Vitals I. Widened pulse pressure II. Bradycardia III. Irregular respirations IV. Eyes do not PERRLA V. Elevate head of the bed to 30 or 45 degrees Parkinson¶s A. Dopamine Hydrocephalus A. II B. 6th nerve defect Meningitis A. 3, 4, 6, 7, 8 Lumber puncture A. Measure pressure in CSF B. Indicate neuro disorders, infections, brain, or spinal cord damage EEG A. Avoid caffeine and hair products before the test II A. Compresses brain structures B. Reduces blood flow C. Widened pulse pressure D. Bradycardia E. Increased temp. F. Cheyne-stokes G. ister oxygen and monitor intake and output H. Elevate head of bed 30-45 degrees Seizures A. Prodromal
I. Mood changes, irritability, insomnia 9. Meniere¶s Disease A. Salt-free diet B. Vasodilators C. Neuroleptics D. Diuretics E. Anti-histamines F. Anti-cholingergics G. Sedatives H. Encourage slow movement 10. Acute closed angle glaucoma A. Severe eye pain B. halos C. Pupils dilate D. nausea and vomiting E. ister stool softeners, constrictive clothing, and colds 11. Detached retina A. Sclera buckling
Cardiovascular 1. Peripheral Vascular Disease A. Arterial I. Arteriosclerosis & Atherosclerosis II. Raynaud, Buerger, and Diabetes diseases III. Smooth, shiny skin with loss of hair IV. Thickened nails V. pale when elevated, rubor when dependent VI. Decreased or absent pulses (impaired perfusion) VII. Sharp pain; intermittent claudicateion VIII. necrotic ulcers on lateral lower legs, toes, and heels IX. cool temperature (reduced blood supply) X. pain is relieved when dependent XI. numbness and tingling (impaired perfusion) Ai I. Anti-platelets to thin blood) ii. anti-hypertensives iii. anti-coagulants iv. exercise B. Venous I. DVT and valvular disorders II. Varicose veins III. venous stasis ulcers iv. brown pigment around ankles v. cyanotic when dependent vi. normal pulses vii. ulcers on medial legs and ankles viii. marked edema ix. elevate extremities for relief x. warm temperature C. Avoid crossing legs and wearing constrictive clothing D. Keep legs dependent if arterial, and elevated if venous E. Compression dressing for venous 2. AAA A. abdominal and back pain (pressure on lumbar nerves) B. Bruit
c c c
C. Asses peripheral pulses (tachycardia and hypotension indicates hemorrhage or shock) D. Neuro (brain is not being perfused) E. Vitals I. Impending shock and graft occlusion F. Renal i. artery clamped×kidney damage ii. BUN and creatnine G. graft occlusion I. change in pulses ii. pain iii. coolness below graft iv. white or blue extremities H. pulsatile mass I. 3. DVT A. calf pain B. edema C. warmth and redness D. tender areas E. Notify doctor of abnormal bleeding during drug therapy F. avoid aspirin G. wear anti-embolism stockings H. anti-coagulants I. elevate leg 4. Valvular disorders A. Decreased cardiac output B. impaired gas exchange C. stenosis or regurgitation D. mitral valve most commonly effected *E. prophylactic treatment before dental work to prevent infection of the heart, and lifelong anticoagulant therapy F. 5. Endocarditis A. vegetation adhere to the valve surface of endocardium B. Fever, chills, malaise, fatigue, splenomegaly, C. Murmur *D. Symptoms of heart failure E. *treat with antibiotics 6. Pericarditis A. friction rub B. substernal pain radiating to back and arm, worst on inspiration, better when leaning forward C. Fever D. Dysphagia (fluid around heart places pressure on esophagus) E. Tachypnea 7. Cardiac tamponade A. JVD (heart is squeezed, so blood backs into circulation) B. hypotension (decreased cardiac output) C. muffled heart sounds (due to fluid accumulation) D. pulsusparadoxius (pulse drops during inspiration) E. decreased LOC F. Increased HR G. edema H. *treat with 02 8. Atherosclerosis
c c c
A. life-style modification B. nitrates C. antihypertensive d. anti-coagulants e. calcium-channel blockers f. ACE inhibitors g. anti-platlets µ 9. Arteriolosclerosis A. arteries harden and thicken B. vitals organs are not adequately perfused C. kidneys are most affected 10. Buerger¶s disease A. inflammation and blockage of small and medium sized arteries of the extremities B. Caused by smoking (causes inflammation and constriction of blood vessels) C. claudication D. numbness and tingling E. skin ulcerations and gangrene 11. How to calculate mean arterial pressure A. (SBP+2DP)/3 i. less than 60 indicates inadequate perfusion 12. PTT a. 16-40 normally 13. Central venous pressure A. 5-10 cm water 14. Stenosis-blood flow is impeded 15. regurgitation-backward leakage of blood 16. Mitral valve disorders (both sided heart failure) 17. Aortic disorders-left side heart failure 18. Avoid green leafy vegetables while taking warfarin 19. APPT with heparin: 60-80 seconds
Gastrointestinal System 1. Hiatal Hernia A. Portion of the stomach protrudes through esophageal hiatus B. Feeling of fullness C. Feeling of suffocation and smoothing after meals (eating distends the stomach, leading to decreased ability of the lungs to expand D. Breathing difficulty E. Anemia F. *sit up after eating 2. GERD A. Pain, burning, and dysphagia (scarring from irritation) B. Eat low fat, high protein foods C. Limit chocolate and mints D. Avoid carbonated beverages E. Proton pump inhibitors (zole) F. H2 receptor blockes (dine) G. Antacids H. mucosal barrier fortifiers (sucralfate-Carafate) I. Can lead to stricture and barret¶s esophagus 3. Peptic ulcer disease
c c c
A. Erosion of the lining of the stomach, pylorus, duodenum, or esophagus due to exposure of hydrocholoric acid, pepsin, and H. pylori infection B. Caused by NSAIDS, alcohol, smoking, anti-coagulants, and trauma C. Belching, bloating, epigastric pain, indigestion, pain after eating, nausea, and vomiting D. Gastric: eating causes pain; Duodenal: eating helps pain Treatments: A. avoid spicy foods B. Give cytotec and other anti-ulcer meds C. Antacids neutralize gastric acid D. Monitor for i. dark, tarry stools (melena) ii. coffee-ground vomit iii. bright red rectal bleeding iv. fatigue v. pallor vi. abdominal pain vii. abdominal mass or bruit viii. decreased BP, rapid pulse, cool extremities Treatments A. saline lavage B. NPO and IV fluids 4. Perforation A. ulcers penetrating the wall of the GI tract B. sudden, excruciating pain in shoulders C. becomes more intense with position change and deep breathing D. Rebound tenderness E. fever Treatments A. ister fluids B. NG suction C. emergency surgery 5. Stomatitis A. ask about nutrition, oral hygiene, antibiotic use, use of mouthwash and toothpaste B. Use soft bristle tooth brushes C. Avoid spicy foods D. Viscous lidocane-can numb throat and impair swallowing E. *risk for impaired nutrition and fluid volume deficit 6. Gastritis (inflammation of stomach lining) A. Pain, heartburn, belching, bloating, loss of appetite, and weight loss, bleeding B. Antacids and anti-biotics due to H. Pylori infection 7. Gastroenteritis A. inflammation of GI tract B. *Diarrhea (large intestine cannot retain fluids): hallmark sign C. abdominal cramps due to inflammation D. loss of appetite E. dehydration due to diarrhea F. weakness and fatigue due to nausea and vomiting G. obtain history of travel and recent foods eaten Treatments A. replacing fluids and electrolytes B. avoid dairy products, vegetables, and fruits
c c c
C. avoid caffeine D. perform skin care due to diarrhea E. avoid raw meat, fruit, and vegetables during travel F. Do not use tap water or ice G. monitor for s/sx of dehydration: decreased urination, dry skin and mucous membranes, dark urine, decreased BP, low potassium and sodium levels, and elevated BUN 8. Malabsorption A. nutrients are digested or absorbed properly B. Weight loss C. steatorrhea due to decreased fat absorption D. diarrhea E. increased bruising F. edema due to decrease protein absorption G. anemia due to vitamin B12, and iron deficiency 9. Polyps A. Bleeding due to polyp irritation B. Abdominal pain and cramping due to obstruction of GI contents C. Diarrhea due to polyp excretion of water and salts Treatments A. polypectomy B. increase calcium intake C. exercise D. low fat, high fiber diet 10. Hemorrhoids A. bleeding due to irritation B. itching due to inadequate cleaning of rectum C. pain Treatments A. sitz bath B. creams and ointments C. compress pads and wiping with moist wipes D. high fiber diet and increase fluids E. stool softener F. avoid long periods of sitting 11. Dumping syndrome A. sweating B. fatigue and desire to lie down C. palpitations D. light-headedness and syncope E. flushing F. abdominal pain and cramping G. hunger Treatments A. restrict fluid during eating B. eat small frequent meals C. lie flat on left side after eating D. decrease carbs and increase fat and proteins E. dietary fiber supplements F. anti-cholinergics 12. Hernia A. Inguninal, femoral, umbilical, and incisional B. caused by increased abdominal pressure and abdominal surgery C. new onset pain and tenderness indicate strangulation D. Decrease abdominal pressure E.provide stool softeners
c c c
F. Avoid coughing post op and increase fluids 13. Intestinal obstruction A. abdominal cramping and pain due to obstruction B. distention because foods or gas cannot the obstruction C. bowel changes D. decreased bowel sounds distal to obstruction E. vomiting due to accumulation of fluids F. fluid and electrolyte imbalances due to inability to absorb nutrients G. Fever due to infection Treatments A. NPO B. NG tube low to suction to remove contents C. Fluid and electrolyte replacement D. withhold pain meds 14. Appendicitis A. pain around umbilical area B. fetal position helps relieve pain C. abdominal guarding D. pain increases with cough and movement and relieved by flexion of knees (rupture) E. nausea and vomiting F. AVOID USING HEAT! G. DO NOT GIVE LAXATIVES OR ENEMAS H. NPO I. IV fluids J. antibiotics 15. Peritonitis (risk for shock) A. inflammation of peritoneum B. pain C. rebound tenderness D. abdominal rigidity E. board like abdomen (widespread inflammation) F. decreased bowel sounds G. increased pulse (hypovolemia) H. decreased urinary output (decreased fluid in circulation) I. nausea and vomiting J. fluid and electrolyte imbalances Treatments A. NPO B. IV fluids and electrolytes C. antibiotics D. NG insertion E. peritoneal lavage to indicate GI bleeding F. oxygen and semi-fowler¶s position *can lead to septicemia, shock, and respiratory distress 16. Crohn¶s disease A. portion of small intestine thickens and narrow the lumen B. Pain, vomiting and diarrhea C. weight loss and malabsorption D. elevate temperature E. fluid and electrolyte imbalances due to malabsorption F. NPO for bowel rest G. low residue diet: low fiber, low fat diet high in calories, carbs, proteins, and vitamins
c c c
H. I. J. K.
corticosteroids anti-diarrheals antibiotics Increase calories and fluids to heal fistulas
17. Ulcerative colitis A. inflammation of large intestine and rectum B. 10-20 liquid stools per day C. rectal bleeding D. increased bowel sounds E. weight loss F. *bloody diarrhea mixed with mucous G. anemia H. NPO I. TPN J. low-residue foods, low-fat, high protein, high calories food K. Avoid milk and encourage bed rest L. anti-diarrheals M. sulasalazine 18. Irritable bowel syndrome A. altered intestinal motility B. diarrhea, constipation, or both C. bloating and gas D. Increase fiber and give laxatives for constipation E. anti-diarrheals and increase fluids for diarrhea F. avoid caffeine, dairy foods, and fructose G. bulk-forming laxatives for constipation H. anti-depressants I. Imodium for diarrhea 19. Diverticulitis A. inflammation or infection of blind pouches B. pain C. fever D. weakness E. diarrhea F. anemia caused by rectal bleeding G. do not do barium enema or colonoscopy during diverticulitis H. liquid diet initially I. low fiber diet J. avoid laxatives K. *signs of intestinal obstruction L. acute phase: NPO or liquids M. recovery: no fiber or foods N. maintenance: high fiber with bulk forming laxatives. Avoid popcorn, nuts, or seeds 20. Ileostomy drains liquid, increasing risk of skin breakdown 21. Pouch system is changed every 3-7 days 22. Cirrhosis A. fatal scarring and fibrosis of liver tissue B. Jaundice due to bilirubin build up C. Pruritis& clay colored stools D. ascites due to decreased albumin (albumin keeps fluid in vascular space) E. hepatomegaly F. nausea due to toxin buildup
c c c
G. spider angiomas (decreased vitamin K) H. increased medication sensitivity I. splenomegaly (decreased platelets and WBCs) J. Esophageal varices (portal hypertension) K. Neuro deficits (increased ammonia buildup): encephalopathy L. shortness of breath M. increased bilirubin, albumin, ALT & AST, PT, serum ammonia Treatments A. take vitaminas B. sodium and fluid restriction C. frequent rest periods D. diuretics E. albumin istration F. elevate head 30 degrees G. monitor meds H. monitor esophageal bleeding 23. Cholecystitis A. inflammation of gallbladder B. pain righting to right shoulder and scapula C. nausea and vomiting due to pain D. fever, elevated liver enzymes, and bilirbun E. steatorrhea&jaunide f. NPO initially G. low fat diet H. anti-spasmodics and anticholinergics I. morphine can cause spasms J. IV hydration and pain control K. decompress stomach with NG tube 24. Pancratitis A. enzymes are activated while still in pancreas B. autodigestion C. Pain radiating to back or epigastrium radiating to left should or back D. decreased bowel sounds E. respiratory distress caused by enzymes entering pleura cavity F. cullen¶s sign (blue color around umbilicus) G. decreased LOC h. turner¶s sign (gray color of flank) I. ascites J. steatorrhea Treatments A. IV fluids and electrolytes B. NPO C. prophylactic antibiotic D. oxygen istration E. NG low to suction F. pain management G. replacement of pancreatic enzymes H. insulin I. measure abdominal girth
OTHER GI NOTES 1. The barium swallow study detect anatomic and functional changes of the esophagus, stomach, and small intestine. A. laxatives and fluids are given after the test 2. The barium enema study detects changes of the large intestine.
c c c
3. Clear liquid diet indicated for endoscopic studies. 4. Monitor cardiac and respiratory functions after EGD procedure 5. Antacids and H2 receptor antagonists should not be given before gastric analysis. A. Pernicous anemia B. Zollinger-Ellison¶s syndrome 6. Place on right side after liver biopsy 7. TPN for GI motility disorders and dysfunction A. check weight and glucose levels B. monitor for infection and air embolism 8. GERD: avoid citrus fruits, caffeine, garlic, fried foods, onions, and tomato-based products 9. Gastric resection (Bilroth I & II): NPO until suture line heals 10. Dumping syndrome: avoid high-carb meals; eat high-protein, high-fat, low carb meals 11. IBS: pain relieved by sleeping and having a bowel movement 12.
13. Hepatitis: focus on prevention
c c c
14. Cirrhosis: normal liver cells are replaced with scar tissue 15. Regular functions of the liver: A. synthesis of clotting factors B. metabolism of hormones (aldosterone, ADH, estrogen and testerone) C. synthesize albumin (maintains normal colloid pressure) D. carb, protein, and fat metabolism E. filtration of drugs F. storage of vitamins and minerals 16. Early stages of cirrhosis: enlarged liver, jaundice, GI disturbances, abdominal discomfort 16.late stages: enlarged spleen, ascites, bleeding tendencies, esophageal varices, dyspnea, pruritis, clay-colored stools 17. end-stage: heptatis encephalopathy 18. Encourage rest, decreased fluid intake, high-calorie, low-protein, lowsodium, low-fat diet, assess abdominal girth, diuretics, lactulose, IV fat soluble vitamins and albumin
c c c
A. low-protein due to the body¶s inability to secrete ammonia, lowsodium to prevent ascites, low-fat diet due to the liver¶s inability to break down fats 19. Varices in the esophagus bleed due to coughing, trauma, and vomiting 20. Murphy sign A. extreme pain on deep inspiration: cholecystitis 21. Greatest risks for pancreatitis are those suffering from alcohol abuse, liver, and gallbladder disease 22. Do not give ice chips and hard candies to prevent stimulation of pancreas 23. Major complication of liver biopsy is hemorrhage, so assess PT prior to procedure 24. GGT assesses possibility of alcohol abuse 25. Fatty foods have no direct effect on diverticulitis 26. Ginger root has antiemetic, analgesic, and sedative properties 27. Bariatric surgery results in the construction of a small pouch in the upper part of the GI. Overfilling of the pouch leads to nausea 28. *Zenker¶s diverticulum is an outpouching of the esophagus near the hypopharyngealspincter. Risk for aspiration 29. Weight can cause a non-alcoholic fatty liver 30. Beta-blockers are given in cirrhosis to prevent esophageal varrices bleeding 31. Positioning the client on the right side after a liver biopsy splints the puncture site to prevent and decrease bleeding. 32. Grey-Turner sign in pancreatitis-blood-stained exudates from the pancreas indicates a severe disease process 33. Patients with IBS have mucous in stools 34. Bowel strictures in Crohn¶s disease can lead to obstruction 35. Patients are placed in side-lying position after anorectal surgery 36. Asprin decreases risk of colon cancer 37. Peristalsis do not return for 3-5 days after abdominal surgery
c c c
DIABETES 1. Type I A. Glucose usually 350 and above B. Ketonuria C. Bicarbonate less than 15 D. Clients are usually thin and under 30 2. Type II. A. *nonketotic hyperosmolar hyperglycemia B. Plasma hyperosmolality C. Dehydration D. change in mental status 3. Assessment: A. Breaks in skin B. Dental caries and fungal infection C. Cataracts and diabetic retinopathy D. Chest pain and shortness of breath E. Hair loss on extremities with non-palpable pulse, pallor, and ulcerations F. Edema of face, hands, feet, and urinary retention G. Neuropathies H. night time diarrhea I. vaginal dryness and frequent yeast infections 4. Take meds according to insulin peak times 5. Eat bedtime snacks 6. Wash feet daily but DO NOT soak! Dry them well 7. Do not moisturize feet between toes 8. Sandles should be avoided 9. Do not wear garters or elastic topped socks 10. Stress and illness can cause hyperglycemia 11. Hypovolemia (polyuria)
Oral meds 1. Sulfonylureas (Glyburide &glipizide) A. stimulates the release of insulin from pancreas and tissues take up glucose more easily B. hypoglycemia is adverse reaction C. Give with meal once daily 2. Biguinides (metformin) A. inhibit hepatic glucose production and increase sensitivity of tissue to insulin B. GI disturbances 3. Thiazolidinediones (actos&avandia) A. decrease insulin resistance to the tissues B. weight gain and edema 4. Alpha-glucosidase inhibitors A. decrease blood glucose absorption B. take with first bite of each meal 5. Meglitindes A. same as sulfonylureas
c c c
*Insulins 1. Rapid acting A. Humalog &Novolog B. 5-15 minutes onset C. 45-1.5 hours peak D. Give within 5-15 minutes of meal 2. Short acting A. Regular insulin B. 30-60 minutes onset C. 2-3 hours peak 3. Intermediate A. NPH &Humulin L B. 1-2 hours onset C. 6-12 hours peak 4. Long acting A. Lantus B. 4-8 hours onset C. 14-20 hours peak D. Give at bedtime E. Bottle is shaped differently than regular insulin, but is clear F. Do not shake or mix with other insulins
1. 2. 3. 4. 5. 6.
Diabetic ketoacidosis Body breaks down fat-×ketones Metabolic acidosis decreased LOC hypovolemia (excess sugar and fluid is excreted) electrolyte imbalances (hyperkalemia) Kussmaul respirations to blow off excess acid
*monitor for hyperglycemia hyperosmolar nonketotic syndrome 1. Extremely high glucose 2. elevated BUN Hypoglycemia 1. soda, orange juice, apple juice, or hard candy 2. complex carbohydrate (half of peanut butter sandwich, milk, and cheese crackers
c c c
Other notes 1. post-pandrial glucose is less than 140 2. A1C: 4-7% 3. Diabetics have increased risk for infection 4. Cool, clammy skin is often seen in hypoglycemia 5. in diabetic ketoacidosis, the skin is flushed due to dehydration and poor skin turgor A. ister IV saline, potassium and insulin 6. A bedtime snack is not needed with long-acting insulin 7. Exercising with glucose levels exceeding 250 and ketonuria increases secretion of glucagon, growth hormone, and catecholamines, casuing the liver to release more glucose
Fluids Imbalances 1. Organs involved: A. kidney (fluid and electrolyte, acid-base balances) B. lungs (acid-base balance, rid 300 ml of fluid) C. heart (kidney perfusion) D. adrenal gland (secrete aldosterone) E. pituitary gland (secrete ADH) F. parathyroid gland 2. Fluid volume deficit: A. loss of water, electrolytes remain normal, but sodium increases) B. Decreased skin turgor C. oliguria D, dry and sticky mucous membranes E. weak, rapid pulse F. Elevated BUN (measures excretory function of kidney) G. elevated Creatnine H. Increased serum osmolarity (amount of solvent is decreased) I. Elevated Hgb and Hct J. Replace isotonic fluids because water is hypotonic K. Strict I & o L. Increased urine osmolality (due to concentrated urine) i. 1.001-1.030 3. Fluid volume excess: A. Body retains water, sodium level decreases B. Heart, renal, liver failure C. Peripheral edema D. bounding pulse with increased BP E. distended neck and hand veins F. dyspnea G. All lab values decreased (hemodilutional state with diluted urine) H. Diuretics I. Fluid and salt restriction J.Strict I & O K. Weigh daily
c c c
Electrolyte Imbalances 1.c Sodium: 135-145 2.c Potassium: 3.5-5 3.c Calcium: 9-10.5 4.c Magnesium: 1.3-2.1 5.c Chloride: 95-105 6.c Phosphate: 3-4.5 Abnormalities and common causes Hyponatremia -diuretics -hypotonic solutions -sweating
Hypernatremia -water deprivation -watery diarrhea -renal failure
Hypokalemia -diuretics -vomiting -NG suctioning
Hyperkalemia -oliguria -renal failure -acidosis
Hypocalcemia -renal failure -hypoparathyrodism -malabsorption
Hypercalcemia
c c c
S/Sx
Treatment
- muscle weakness (decreased excitability of cell membranes) -seizures -muscle cramps -twitching -lethargy and confusion Thirst -tachycardia (heart is trying to pump around what little fluid is left) -dry mouth -irritability -muscle weakness (potassium is needed for muscle contraction) -decreased GI motility -dysrhythmias -paresthesia -slow, difficult respirations (respiratory muscles are weak) -bradycardia -dysrhythmias -flaccid paralysis (excessive potassium interferes with muscle contraction) -diarrhea -numbness and cramps -tingling of extremities -convulsions (muscles contract) -positive trousseau sign (hyperexcitability of hand muscles) -positive chvostek¶s sign (hyperexcitabilty of facial muscles) -laryngeal spasms -increased DTRs -constipation
-restrict fluids -hypotonic or hypertonic saline solutions -increase dietary sodium
-restrict sodium -increase water intake
-never give bolus (do not exceed 20 meq) -assess renal status before istration -eat bananas, oranges, cantaloupes, avocados, spinach, potatoes -ister potassium chloride ister 50% glucose with regular insulin -ister kayexalate -ister calcium gluconate -IV loop diuretics -ister calcium IV slowly -vitamin D
-ister
-hyperparathyroidism
-polyuria -polydipsia -dysrhythmmias -respiratory arrest (sedative respiratory muscles) -decreased bowel sounds (intestines are sedated) -muscle weakness (sedated muscles)
calcitonin(moves calcium into the bones) -IV phosphate
Hypomagnesemia -alcoholism -diabetic ketoacidosis -malabsorption
same signs and symptoms of hypercalcemia -BP increases (vasoconstriction)
-ister magnesium sulfate
Hypermagnesemia -renal failure
-flushing -hypotension -drowsiness -depressed respirations -hypoactive reflexes -bradycardia -BP decreases (vasodilation) -facial flushing and warming (vasodilation) -sedated respiratory muscles -parestheias -muscle weakness -cardiomyopathy -respiratory failure -(SIGNS AND SYMPTOMS OF HYPERCALCEMIA) -tentanysymptons (SIGNS AND SYMPTOMS OF HYPOCALCEMIA)
Avoid magnesium based antacids and laxatives -0.45 saline solution -IV calcium gluconate -loop diuretics -respiratory
Hypophosphaemia -alcohol withdrawal
Hyperphosphatemia -renal failure
-IV phosphorus when serum level drops below 1
ister aluminum hydroxide -ister vitamin D
Other notes 1. hyponatremia caused by hypervolemia: fluid restriction
c c c
Acid-base balance 1. 20 bicarbonate to 1 carbonic acid ratio 2. Respiratory acidosis A. Pulmonary disease B. Sleep apnea 3. Respiratory alkalosis A. over-ventilation B. response to hypoxia C. fever 4. Metabolic acidosis A. lactic acidosis B. ketoacidosis C. acid ingestion 5. Metabolic alkalosis A. Gastric drainage B. vomiting C. burns
Peri-operative 1. Surgical risks A. young and old B. obese and malnourished C. dehydrated D. clients with any infection E. cardiac conditions F. blood coagulation disorders G. upper respiratory tract infections and COPD H. renal disease (renal insufficiency) I. diabetes due to delayed healing and possibility of wound infection J. Use of anticoagulants K. use of antibiotics (may be incompatible to anesthesia) L. diuretic use (electrolyte imbalances) M. steroids N. vitamin E use 2. Client has to be 18 to sign surgical consent form c Pre-operative 1. Client teaching: A. Coughing and deep breathing B. ing the wound by splinting C. leg exercises D. Turning, positioning, ambulation E. Recovery room procedures F. Type of dressing, NG tubes, drains, foley catheter G. Decreases anxiety and promotes client participation H. Regulations about jewelry I. NPO status J. Dietary restrictions K. informed consent must be signed before the istration of medications
c c c
Intra-operative 1. report changes in pulse, temperature, respirations, and blood pressure to surgeon . Postoperative 1. Signs A. B. C. D.
of shock and hemorrhage hypotension tachycardia narrowed pulse pressure cold, moist skin
2. Post-op care A. Pulmonary i. Airway (check gag reflex) ii. Bilateral breath sounds iii. Deep breathing and coughing B. Neuro i. LOC ii. Reflexes C. Circulation i. Vital signs ii. Peripheral perfusion D. GI i. Bowel sounds ii. Distention E. GU i. Urinary output ii. Intake and output *malignant hyperthermia *somogyi/dawn effect *smoking-pack years
c c c
c c c