This document was ed by and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this report form. Report 2z6p3t
Overview 5o1f4z
& View 1. External & Internal Generative Organs Organs as PDF for free.
More details 6z3438
- Words: 2,820
- Pages: 78
MATERNAL ANATOMY External and Internal Generative Organs
FEU-NRMF Department of Obstetrics and Gynecology
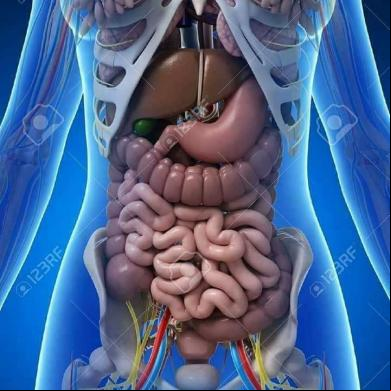
ANTERIOR ABDOMINAL WALL • confines abdominal viscera • stretches to accommodate the expanding uterus • provides surgical access to the internal reproductive organs
ANTERIOR ABDOMINAL WALL
ANTERIOR ABDOMINAL WALL
Skin • LANGER LINES • describe the orientation of dermal fibers • In the abdomen: • Transversely arranged
• vertical skin incisions • more tension, wider scars
• low transverse incisions (Pfannenstiel) • follow Langer lines; superior cosmetic results
Subcutaneous Layer Camper’s fascia › Superficial › predominantly fatty layer
Scarpa’s fascia › Deeper › more membranous layer These are not discrete layers but instead represent a continuum of the subcutaneous tissue layer.
Rectus Sheath
• fibrous aponeuroses of the external oblique, internal oblique, and transversus abdominis muscles in the midline
Arcuate Line Cephalad- aponeuroses invest the rectus abdominis bellies above and below
Caudal- all aponeuroses lie anterior to the rectus abdominis muscle, and only the thin transversalis fascia and peritoneum lie beneath.
Blood Supply
Blood Supply A. Femoral Artery Branches arteries – supply the skin and subcutaneous layers of the anterior abdominal wall and mons pubis › superficial epigastric › superficial circumflex iliac › external pudendal
B. External Iliac Artery Branches - supply the muscles and fascia of the anterior abdominal wall › inferior "deep" epigastric vessels › deep circumflex iliac vessels-.
Hesselbach triangle Boundaries: Inferiorly: inguinal ligament Medially: lateral border of the rectus muscles Laterally: inferior epigastric vessels.
Hesselbach triangle CLINICAL SIGNIFICANCE: Direct hernias-
involves the Hesselbach triangle Indirect hernias-
involves the deep inguinal ring
Anterior Abdominal Wall Innervation Intercostal nerves (T7-11) Subcostal nerve (T12) Iliohypogastric nerve- skin over suprapubic area Ilioinguinal nerves (L1)› skin of the lower abdominal wall › upper portion of the labia majora › medial portion of the thigh T10 dermatome- approximates the level of the umbilicus.
Clinical Significance ILIOINGUINAL AND ILIOHYPOGASTRIC NERVES • can be entrapped during closure of low transverse incisions, especially if incisions extend beyond the lateral borders of the rectus muscle
• carry sensory information only, and injury leads to loss of sensation within the areas supplied.
EXTERNAL GENERATIVE ORGANS
EXTERNAL GENERATIVE ORGANS PUDENDA or VULVA includes all structures visible externally from the pubis to the perineum: Mons pubis Labia majora and minora Clitoris Hymen Vestibule Urethral opening Various glandular and vascular structures
EXTERNAL GENERATIVE ORGANS MONS PUBIS • Also called mons veneris • fat-filled cushion that lies over the symphysis pubis • At puberty, covered by curly hair that forms the escutcheon • In adult women, it is distributed in a triangular area Base: forms the upper margin of the symphysis pubis
EXTERNAL GENERATIVE ORGANS LABIA MAJORA
• Male homologue: scrotum • It is where the round ligaments terminate (upper boarder) • Outer surface with hair while inner surface without hairs • In children and nulliparous women close apposition • In multiparous women - gapes widely
• continuous directly with the mons pubis • Merge posteriorly to form the posterior commissure.
EXTERNAL GENERATIVE ORGANS
LABIA MINORA
composed of connective tissue with many vessels and some smooth muscular fibers moist and reddish, similar in appearance to a mucous membrane extremely sensitive because its supplied with many nerve endings 2 lamellae superiorly lower pair: forms the frenulum of the clitoris upper pair: forms the prepuce Inferiorly, it forms the fourchette.
EXTERNAL GENERATIVE ORGANS LABIA MAJORA • Lining epithelium Outer and Lateral portion of inner surface- stratified squamous epithelium Medial portion- non-keratinized squamous epithelium Hart line- demarcation line between lateral and midline portion
Contains sebaceous follicles, few sweat glands Lack hair follicles, eccrine glands and apocrine glands
EXTERNAL GENERATIVE ORGANS CLITORIS • Male homologue: penis • composed of a glans, a corpus, and two crura • rarely exceeds 2 cm in length. • covered by stratified squamous epithelium that is richly supplied with nerve ending • principal female erogenous organ
EXTERNAL GENERATIVE ORGANS VESTIBULE • from embryonic urogenital membrane
• almond-shaped • BOUNDARIES: • Lateral- Hart line • Medial – external surface of hymen • Anteriorly- frenulum • Posteriorly- fourchette
EXTERNAL GENERATIVE ORGANS VESTIBULE • 6 openings: • urethra • vagina • ducts of the Bartholin glands (2) • ducts of the paraurethral glands/skene glands (2)
Vestibular Glands BARTHOLIN’S GLANDS • greater vestibular glands • 0.5 to 1 cm in diameter • lie inferior to the vestibular bulbs and deep to the inferior ends of the bulbocavernosus muscle • ducts are 1.5 to 2 cm long and open distal to the hymenal ring at 5 & 7 o'clock
Vestibular Glands BARTHOLIN’S GLANDS CLINICAL SIGNIFICANCE: • Following trauma or infection, either duct may swell and obstruct to form a cyst, or if infected, an abscess
Vestibular Glands PARAURETHRAL GLANDS • Lies in the inferior aspect of the urethra • Skene glands - largest • Minor vestibular glands - are shallow glands lined by simple mucin-secreting epithelium and open along Hart line.
Vestibular Glands PARAURETHRAL GLANDS CLINICAL SIGNIFICANCE: • Inflammation and duct obstruction of any of the paraurethral glands can lead to a urethral diverticulum formation.
Vestibular Bulbs • Male homologue: corpus spongiosum of the penis • almond-shaped, mainly composed of aggregations of veins • 3 to 4 cm long, 1 to 2 cm wide, and 0.5 to 1 cm thick
• lie beneath the bulbocavernosus muscle on either side of the vestibule.
Bulbocavernosus muscle
Vestibular bulb
Vestibular Bulbs CLINICAL SIGNIFICANCE: • During childbirth, the vestibular bulbs may be injured and may even rupture to create a vulvar hematoma
VAGINAL OPENING AND HYMEN Vaginal opening is rimmed distally by the hymen or its remnants
VAGINAL OPENING AND HYMEN HYMEN • Membrane surrounding the vaginal opening • Composed of elastic and collagenous connective tissue • Covered by stratified squamous epithelium
VAGINAL OPENING AND HYMEN • The aperture of the hymen varies. • Hymen is torn at several sites during first coitus. Identical tears may occur by other penetration. The edges of the torn hymen soon reepithelialize hymenal caruncle • Imperforate hymen • Rare lesion in which the vaginal orifice is occluded completely, causing retention of menstrual blood
VAGINAL OPENING AND HYMEN VAGINA • Musculo-membranous structure • Extends from the vulva to the uterus • interposed anteriorly and posteriorly between the urinary bladder and the rectum . • Lining epithelium: nonkeratinized stratified squamous epithelium • no glands • abundant vascular supply
VAGINAL OPENING AND HYMEN VAGINA Embryology upper portion - müllerian ducts lower portion - urogenital sinus
VAGINAL OPENING AND HYMEN VAGINA Anteriorly, the vagina is separated from the bladder and urethra by connective called – vesicovaginal septum
Posteriorly, there are similar tissues together that form the rectovaginal septum between the lower portion of the vagina and the rectum The upper fourth of the vaginal is separated from the rectum by the rectouterine pouch or culdesac of Douglas
VAGINAL OPENING AND HYMEN
VAGINA • Length • •
Anterior: 6 – 8cm Posterior: 7 – 10cm
• Subdivided by the cervix into fornices anterior, posterior, lateral
VAGINAL OPENING AND HYMEN VAGINA •
•
The fornices are clinically important because the internal pelvic organs can be palpated through their thin walls Posterior fornix provides surgical access to the peritoneal cavity
VAGINAL OPENING AND HYMEN VAGINA BLOOD SUPPLY
Upper Third Middle third Lower third
cervicovaginal branches of uterine artery and vaginal artery inferior vesical arteries middle rectal and internal pudendal arteries
LYMPHATIC DRAINAGE
Externa, internal and common iliac nodes Internal iliac nodes Inguinal nodes
PERINEUM The diamond area between the thighs Boundaries are same as those of the bony pelvic outlet
Anterior: Pubic symphysis Posterior: Ischiopubic rami Anterolateral: Ischial tuberosities Posterolateral: Sacrotuberous ligaments Posterior: Coccyx
Blood supply: Internal pudendal artery (inferior rectal artery and posterior labial artery)
Anterior triangle, also called the urogenital triangle
Posterior triangle, also called the anal triangle
Ischial Tuberosities – divides the perineum into an anterior and posterior triangle
PERINEUM ANTERIOR TRIANGLE Also called Urogenital Triangle Further subdivided into: Superficial space – closed compartment Deep space – continuous superiorly with the pelvic cavity
Boundaries: Superior: Pubic rami Lateral: Ischial tuberosities Posterior: Superficial transverse pernieal muscle
PERINEUM
PERINEUM SUPERFICIAL SPACE OF THE ANTERIOR TRIANGLE Ischiocavernosus
• attached at the ischial tuberosity and crus of clitoris helps maintain clitoral erection
Bulbocavernosus
• Overly the vestibular bulb and Bartholin glands • Attached at the perineal body and the clitoris • Constrict the vaginal lumen and aid in the release of secretions of the Bartholin’s gland • Contributes to clitoral erection
Superficial transverse perineal muscles
• attach to the ischial tuberosities laterall and the perineal body medially
PERINEUM DEEPSPACE OF THE ANTERIOR TRIANGLE • Deep to the perineal membrane and extends up continuous superiorly with the pelvic cavity • Contains: compressor urethrae, urethrovaginal sphincter muslces, external urethral sphincter, parts of urethra and vagina, branches of internal pudendal artery, dorsal nerve and vein of the clitoris
PERINEUM POSTERIOR TRIANGLE Contains: Ischiorectal fossa Anal canal Anal sphincter complex Branches of the internal pudendal vessels Pudendal nerve
POSTERIOR TRIANGLE Ischiorectal fossae • Two fat filled wedge shaped spaces on either side of the anal canal • Provide to surrounding structures, yet allow distension of the rectum during defecation and stretching of the vagina during delivery • Anal canal and sphincter lie in the center of the fossae. • This continuity of the fossae across perineal compartments allows fluid, infection and malignancy to spread.
PERINEUM
PERINEUM PUDENDAL NERVE • Formed by the anterior rami of S2-S4 • Lies posteromedial to the ischial spines
PERINEUM PUDENDAL NERVE •3 terminal branches: • Dorsal nerve of the clitoris – supplies the skin of the clitoris • Perineal nerve – supplies the muscles of the anterior triangle and labial skin • Inferior rectal nerve – supplies the external anal sphincter, mucous membrane of anal canal and the perineal skin
Anus EXTERNAL ANAL SPHINCTERS • A ring of striated muscle attached to the perineal body anteriorly and the coccyx posteriorly • Maintains the constant state of resting contraction • Receives blood supply from the inferior rectal artery • Motor fibers come from the inferior rectal branch of the pudendal nerve
Anus INTERNAL ANAL SPHINCTER • Contributes the bulk of the anal canal resting pressure for fecal continence • Formed by the distal continuation of the inner circular muscle layer of the rectum and colon
ANAL CUSHION • Highly vascularized • Aids in fecal continence • Engorgement due to increased uterine size, excessive straining and hard stools, can increase venous engorgement within these cushions to form hemorrhoids
Perineal body Structures that contribute to the perineal body: • Median raphe of the levator ani • Central tendon of the perineum • Bulbocavernosus m. • Superficial transverse perineal m. • External anal sphincter
INTERNAL GENERATIVE ORGANS
Development of the internal generative organs
Embryological development Fusion of the two müllerian (paramesonephric) ducts to form a single canal begins at the level of the inguinal crest, that is, the gubernaculum (primordium of the round ligament) – 5th week of development Upper ends of the müllerian ducts produce the oviducts and the fused parts give rise to the uterus The vaginal canal is not patent throughout its entire length until the sixth month of fetal life
INTERNAL GENERATIVE ORGANS
Cervix Internal cervical os upper boundary; level at which the peritoneum is reflected up onto the bladder
Portio supravaginalis • is covered by peritoneum on its posterior surface • attached to the cardinal ligaments laterally
Portio vaginalis
INTERNAL GENERATIVE ORGANS Cervix External cervical os before childbirth: small, oval opening External cervical os after childbirth: transverse slit, giving rise to the anterior and posterior cervical lip Cervical stroma – compose mainly of collagen, elastin and proteoglycan but very little smooth muscle Ectocervix – nonkeratinized squamous epithelium Endocervix – mucin-secreting columnar epithelium
INTERNAL GENERATIVE ORGANS
Uterus
Thick- walled, hollow, muscular organ Nulliparous: 6- 8cm, fundus and cervix almost equal in length Multiparous: 9-10cm, cervix is 1/3 of the total length Entire posterior wall of the uterus is covered by serosa, or peritoneum, the lower portion of which forms the anterior boundary of the recto-uterine culde-sac, or pouch of Douglas. Blood supply: uterine artery ovarian artery
INTERNAL GENERATIVE ORGANS Uterus: Parts • Corpus or body • Cervix • Isthmus – between the internal cervical os and the endometrial cavity; forms the lower uterine segment during pregnancy • Cornua – at the junction of the superior and lateral margins • Fundus – convex upper segment between the points of insertion of the fallopian tubes
INTERNAL GENERATIVE ORGANS Uterus • Layers: • serosa • muscular (myometrium) • mucosa (endometrium)
• The serosal layer is formed by the peritoneum that covers the uterus
INTERNAL GENERATIVE ORGANS Uterus: Myometrium • Bundles of smooth muscle united by connective tissue in which there are many elastic fibers • Relative more muscle in the inner wall than the outer wall, and in the anterior and posterior walls than in the lateral walls • Muscle fibers diminish caudally such that the muscle comprises only 10% of the tissue mass in the cervix • The interlacing myometrial fibers that surround the myometrial vessels are integral to control of bleeding from the placental site during the third stage of labor
INTERNAL GENERATIVE ORGANS Uterus: Endometrium thin, pink, velvet-like membrane perforated by a large number of minute ostia of the uterine glands. Histology Epithelium - single layer of closely packed high columnar cells than rests on a thin basement membrane Uterine glands – invaginations of the epithelieum that extend to the myometrium Interglandular mesenchymal stroma – varies remarkably throughout the ovarian cycle, undergoes decidualization following ovulation
INTERNAL GENERATIVE ORGANS Uterus: Blood supply
INTERNAL GENERATIVE ORGANS Uterus: Endometrium Vascular architecture • Uterine and ovarian arteries arcuate arteries radial arteries spiral/coiled arteries and basal/straight arteries • Spiral arteries – midportion and superficial third of the endometrium, responsive to hormones • Basal arteries – basal layer, not responsive to hormones
INTERNAL GENERATIVE ORGANS ROUND LIGAMENTS Extend from the lateral portion of the uterus Arise below and anterior to the origin of the oviducts. Terminate in the upper portion of the labium majus. Sampson artery runs within this ligament. Corresponds embryologically to the gubernaculum testis of men Clinically significant when doing puerperal tubal sterilization
INTERNAL GENERATIVE ORGANS BROAD LIGAMENTS • Winglike structures from lateral margins to pelvic sidewall • Each consist of an anterior leaf and a posterior leaf • Drapes over structures extending from the cornu • Mesosalpinx, mesoteres, mesovarium, mesometrium • Suspensory ligament or infundibulopelvic ligament – from the fimbriated end of the fallopian tube to the pelvic wall, where ovarian vessels traverse
INTERNAL GENERATIVE ORGANS CARDINAL LIGAMENTS Transverse cervical or Mackendrodt ligament Thick base of the broad ligament that is continuous with the connective tissue of the pelvic floor
INTERNAL GENERATIVE ORGANS UTEROSACRAL LIGAMENTS • From its attachment posterolaterally to the supravaginal portion of the cervix and inserts into the fascia over the sacram • Form the lateral boundaries of the pouch of Douglas
INTERNAL GENERATIVE ORGANS LYMPHATICS • Cervix • terminate mainly in the hypogastric nodes, which are situated near the bifurcation of the common iliac vessels.
• Body of the uterus • internal iliac nodes and periaortic lymph nodes
Blood Vessels
INTERNAL GENERATIVE ORGANS FALLOPIAN TUBES Also called oviducts Vary in length from 8 to 14 cm. lumen is lined by mucous membrane. PARTS interstitial portion isthmus ampulla infundibulum or fimbriated extremity- funnel-shaped opening at the distal
INTERNAL GENERATIVE ORGANS FALLOPIAN TUBES •
•
•
Tubal smooth muscle: inner circular and outer longitudinal, undergo rhythmic contraction or peristalsis toward the uterine cavity Epithelium in close with muscle layer because there is no submucosa Epithelium - columnar cells (some ciliated, others secretory)
INTERNAL GENERATIVE ORGANS Ovaries the ovaries vary considerably in size. During childbearing years, they are from 2.5 to 5 cm in length, 1.5 to 3 cm in breadth, and 0.6 to 1.5 cm in thickness. After menopause, ovarian size diminishes remarkably.
Rest in a slight depression on the lateral wall of the pelvis, called ovarian fossa of Waldeyer between the divergent external and internal iliac vessels Attached to the broad ligament by the mesovarium.
INTERNAL GENERATIVE ORGANS Ovaries PARTS: • Cortex- outer layer, contains oocytes and developing follicles • Medulla- central portion, composed of loose connective tissue BLOOD SUPPLY • The ovaries are supplied with both sympathetic nerves from the ovarian plexus and parasympathetic nerves.
THANK YOU!
Quiz
12 13
14,15 – Blood supply to the uterus
Quiz
FEU-NRMF Department of Obstetrics and Gynecology
ANTERIOR ABDOMINAL WALL • confines abdominal viscera • stretches to accommodate the expanding uterus • provides surgical access to the internal reproductive organs
ANTERIOR ABDOMINAL WALL
ANTERIOR ABDOMINAL WALL
Skin • LANGER LINES • describe the orientation of dermal fibers • In the abdomen: • Transversely arranged
• vertical skin incisions • more tension, wider scars
• low transverse incisions (Pfannenstiel) • follow Langer lines; superior cosmetic results
Subcutaneous Layer Camper’s fascia › Superficial › predominantly fatty layer
Scarpa’s fascia › Deeper › more membranous layer These are not discrete layers but instead represent a continuum of the subcutaneous tissue layer.
Rectus Sheath
• fibrous aponeuroses of the external oblique, internal oblique, and transversus abdominis muscles in the midline
Arcuate Line Cephalad- aponeuroses invest the rectus abdominis bellies above and below
Caudal- all aponeuroses lie anterior to the rectus abdominis muscle, and only the thin transversalis fascia and peritoneum lie beneath.
Blood Supply
Blood Supply A. Femoral Artery Branches arteries – supply the skin and subcutaneous layers of the anterior abdominal wall and mons pubis › superficial epigastric › superficial circumflex iliac › external pudendal
B. External Iliac Artery Branches - supply the muscles and fascia of the anterior abdominal wall › inferior "deep" epigastric vessels › deep circumflex iliac vessels-.
Hesselbach triangle Boundaries: Inferiorly: inguinal ligament Medially: lateral border of the rectus muscles Laterally: inferior epigastric vessels.
Hesselbach triangle CLINICAL SIGNIFICANCE: Direct hernias-
involves the Hesselbach triangle Indirect hernias-
involves the deep inguinal ring
Anterior Abdominal Wall Innervation Intercostal nerves (T7-11) Subcostal nerve (T12) Iliohypogastric nerve- skin over suprapubic area Ilioinguinal nerves (L1)› skin of the lower abdominal wall › upper portion of the labia majora › medial portion of the thigh T10 dermatome- approximates the level of the umbilicus.
Clinical Significance ILIOINGUINAL AND ILIOHYPOGASTRIC NERVES • can be entrapped during closure of low transverse incisions, especially if incisions extend beyond the lateral borders of the rectus muscle
• carry sensory information only, and injury leads to loss of sensation within the areas supplied.
EXTERNAL GENERATIVE ORGANS
EXTERNAL GENERATIVE ORGANS PUDENDA or VULVA includes all structures visible externally from the pubis to the perineum: Mons pubis Labia majora and minora Clitoris Hymen Vestibule Urethral opening Various glandular and vascular structures
EXTERNAL GENERATIVE ORGANS MONS PUBIS • Also called mons veneris • fat-filled cushion that lies over the symphysis pubis • At puberty, covered by curly hair that forms the escutcheon • In adult women, it is distributed in a triangular area Base: forms the upper margin of the symphysis pubis
EXTERNAL GENERATIVE ORGANS LABIA MAJORA
• Male homologue: scrotum • It is where the round ligaments terminate (upper boarder) • Outer surface with hair while inner surface without hairs • In children and nulliparous women close apposition • In multiparous women - gapes widely
• continuous directly with the mons pubis • Merge posteriorly to form the posterior commissure.
EXTERNAL GENERATIVE ORGANS
LABIA MINORA
composed of connective tissue with many vessels and some smooth muscular fibers moist and reddish, similar in appearance to a mucous membrane extremely sensitive because its supplied with many nerve endings 2 lamellae superiorly lower pair: forms the frenulum of the clitoris upper pair: forms the prepuce Inferiorly, it forms the fourchette.
EXTERNAL GENERATIVE ORGANS LABIA MAJORA • Lining epithelium Outer and Lateral portion of inner surface- stratified squamous epithelium Medial portion- non-keratinized squamous epithelium Hart line- demarcation line between lateral and midline portion
Contains sebaceous follicles, few sweat glands Lack hair follicles, eccrine glands and apocrine glands
EXTERNAL GENERATIVE ORGANS CLITORIS • Male homologue: penis • composed of a glans, a corpus, and two crura • rarely exceeds 2 cm in length. • covered by stratified squamous epithelium that is richly supplied with nerve ending • principal female erogenous organ
EXTERNAL GENERATIVE ORGANS VESTIBULE • from embryonic urogenital membrane
• almond-shaped • BOUNDARIES: • Lateral- Hart line • Medial – external surface of hymen • Anteriorly- frenulum • Posteriorly- fourchette
EXTERNAL GENERATIVE ORGANS VESTIBULE • 6 openings: • urethra • vagina • ducts of the Bartholin glands (2) • ducts of the paraurethral glands/skene glands (2)
Vestibular Glands BARTHOLIN’S GLANDS • greater vestibular glands • 0.5 to 1 cm in diameter • lie inferior to the vestibular bulbs and deep to the inferior ends of the bulbocavernosus muscle • ducts are 1.5 to 2 cm long and open distal to the hymenal ring at 5 & 7 o'clock
Vestibular Glands BARTHOLIN’S GLANDS CLINICAL SIGNIFICANCE: • Following trauma or infection, either duct may swell and obstruct to form a cyst, or if infected, an abscess
Vestibular Glands PARAURETHRAL GLANDS • Lies in the inferior aspect of the urethra • Skene glands - largest • Minor vestibular glands - are shallow glands lined by simple mucin-secreting epithelium and open along Hart line.
Vestibular Glands PARAURETHRAL GLANDS CLINICAL SIGNIFICANCE: • Inflammation and duct obstruction of any of the paraurethral glands can lead to a urethral diverticulum formation.
Vestibular Bulbs • Male homologue: corpus spongiosum of the penis • almond-shaped, mainly composed of aggregations of veins • 3 to 4 cm long, 1 to 2 cm wide, and 0.5 to 1 cm thick
• lie beneath the bulbocavernosus muscle on either side of the vestibule.
Bulbocavernosus muscle
Vestibular bulb
Vestibular Bulbs CLINICAL SIGNIFICANCE: • During childbirth, the vestibular bulbs may be injured and may even rupture to create a vulvar hematoma
VAGINAL OPENING AND HYMEN Vaginal opening is rimmed distally by the hymen or its remnants
VAGINAL OPENING AND HYMEN HYMEN • Membrane surrounding the vaginal opening • Composed of elastic and collagenous connective tissue • Covered by stratified squamous epithelium
VAGINAL OPENING AND HYMEN • The aperture of the hymen varies. • Hymen is torn at several sites during first coitus. Identical tears may occur by other penetration. The edges of the torn hymen soon reepithelialize hymenal caruncle • Imperforate hymen • Rare lesion in which the vaginal orifice is occluded completely, causing retention of menstrual blood
VAGINAL OPENING AND HYMEN VAGINA • Musculo-membranous structure • Extends from the vulva to the uterus • interposed anteriorly and posteriorly between the urinary bladder and the rectum . • Lining epithelium: nonkeratinized stratified squamous epithelium • no glands • abundant vascular supply
VAGINAL OPENING AND HYMEN VAGINA Embryology upper portion - müllerian ducts lower portion - urogenital sinus
VAGINAL OPENING AND HYMEN VAGINA Anteriorly, the vagina is separated from the bladder and urethra by connective called – vesicovaginal septum
Posteriorly, there are similar tissues together that form the rectovaginal septum between the lower portion of the vagina and the rectum The upper fourth of the vaginal is separated from the rectum by the rectouterine pouch or culdesac of Douglas
VAGINAL OPENING AND HYMEN
VAGINA • Length • •
Anterior: 6 – 8cm Posterior: 7 – 10cm
• Subdivided by the cervix into fornices anterior, posterior, lateral
VAGINAL OPENING AND HYMEN VAGINA •
•
The fornices are clinically important because the internal pelvic organs can be palpated through their thin walls Posterior fornix provides surgical access to the peritoneal cavity
VAGINAL OPENING AND HYMEN VAGINA BLOOD SUPPLY
Upper Third Middle third Lower third
cervicovaginal branches of uterine artery and vaginal artery inferior vesical arteries middle rectal and internal pudendal arteries
LYMPHATIC DRAINAGE
Externa, internal and common iliac nodes Internal iliac nodes Inguinal nodes
PERINEUM The diamond area between the thighs Boundaries are same as those of the bony pelvic outlet
Anterior: Pubic symphysis Posterior: Ischiopubic rami Anterolateral: Ischial tuberosities Posterolateral: Sacrotuberous ligaments Posterior: Coccyx
Blood supply: Internal pudendal artery (inferior rectal artery and posterior labial artery)
Anterior triangle, also called the urogenital triangle
Posterior triangle, also called the anal triangle
Ischial Tuberosities – divides the perineum into an anterior and posterior triangle
PERINEUM ANTERIOR TRIANGLE Also called Urogenital Triangle Further subdivided into: Superficial space – closed compartment Deep space – continuous superiorly with the pelvic cavity
Boundaries: Superior: Pubic rami Lateral: Ischial tuberosities Posterior: Superficial transverse pernieal muscle
PERINEUM
PERINEUM SUPERFICIAL SPACE OF THE ANTERIOR TRIANGLE Ischiocavernosus
• attached at the ischial tuberosity and crus of clitoris helps maintain clitoral erection
Bulbocavernosus
• Overly the vestibular bulb and Bartholin glands • Attached at the perineal body and the clitoris • Constrict the vaginal lumen and aid in the release of secretions of the Bartholin’s gland • Contributes to clitoral erection
Superficial transverse perineal muscles
• attach to the ischial tuberosities laterall and the perineal body medially
PERINEUM DEEPSPACE OF THE ANTERIOR TRIANGLE • Deep to the perineal membrane and extends up continuous superiorly with the pelvic cavity • Contains: compressor urethrae, urethrovaginal sphincter muslces, external urethral sphincter, parts of urethra and vagina, branches of internal pudendal artery, dorsal nerve and vein of the clitoris
PERINEUM POSTERIOR TRIANGLE Contains: Ischiorectal fossa Anal canal Anal sphincter complex Branches of the internal pudendal vessels Pudendal nerve
POSTERIOR TRIANGLE Ischiorectal fossae • Two fat filled wedge shaped spaces on either side of the anal canal • Provide to surrounding structures, yet allow distension of the rectum during defecation and stretching of the vagina during delivery • Anal canal and sphincter lie in the center of the fossae. • This continuity of the fossae across perineal compartments allows fluid, infection and malignancy to spread.
PERINEUM
PERINEUM PUDENDAL NERVE • Formed by the anterior rami of S2-S4 • Lies posteromedial to the ischial spines
PERINEUM PUDENDAL NERVE •3 terminal branches: • Dorsal nerve of the clitoris – supplies the skin of the clitoris • Perineal nerve – supplies the muscles of the anterior triangle and labial skin • Inferior rectal nerve – supplies the external anal sphincter, mucous membrane of anal canal and the perineal skin
Anus EXTERNAL ANAL SPHINCTERS • A ring of striated muscle attached to the perineal body anteriorly and the coccyx posteriorly • Maintains the constant state of resting contraction • Receives blood supply from the inferior rectal artery • Motor fibers come from the inferior rectal branch of the pudendal nerve
Anus INTERNAL ANAL SPHINCTER • Contributes the bulk of the anal canal resting pressure for fecal continence • Formed by the distal continuation of the inner circular muscle layer of the rectum and colon
ANAL CUSHION • Highly vascularized • Aids in fecal continence • Engorgement due to increased uterine size, excessive straining and hard stools, can increase venous engorgement within these cushions to form hemorrhoids
Perineal body Structures that contribute to the perineal body: • Median raphe of the levator ani • Central tendon of the perineum • Bulbocavernosus m. • Superficial transverse perineal m. • External anal sphincter
INTERNAL GENERATIVE ORGANS
Development of the internal generative organs
Embryological development Fusion of the two müllerian (paramesonephric) ducts to form a single canal begins at the level of the inguinal crest, that is, the gubernaculum (primordium of the round ligament) – 5th week of development Upper ends of the müllerian ducts produce the oviducts and the fused parts give rise to the uterus The vaginal canal is not patent throughout its entire length until the sixth month of fetal life
INTERNAL GENERATIVE ORGANS
Cervix Internal cervical os upper boundary; level at which the peritoneum is reflected up onto the bladder
Portio supravaginalis • is covered by peritoneum on its posterior surface • attached to the cardinal ligaments laterally
Portio vaginalis
INTERNAL GENERATIVE ORGANS Cervix External cervical os before childbirth: small, oval opening External cervical os after childbirth: transverse slit, giving rise to the anterior and posterior cervical lip Cervical stroma – compose mainly of collagen, elastin and proteoglycan but very little smooth muscle Ectocervix – nonkeratinized squamous epithelium Endocervix – mucin-secreting columnar epithelium
INTERNAL GENERATIVE ORGANS
Uterus
Thick- walled, hollow, muscular organ Nulliparous: 6- 8cm, fundus and cervix almost equal in length Multiparous: 9-10cm, cervix is 1/3 of the total length Entire posterior wall of the uterus is covered by serosa, or peritoneum, the lower portion of which forms the anterior boundary of the recto-uterine culde-sac, or pouch of Douglas. Blood supply: uterine artery ovarian artery
INTERNAL GENERATIVE ORGANS Uterus: Parts • Corpus or body • Cervix • Isthmus – between the internal cervical os and the endometrial cavity; forms the lower uterine segment during pregnancy • Cornua – at the junction of the superior and lateral margins • Fundus – convex upper segment between the points of insertion of the fallopian tubes
INTERNAL GENERATIVE ORGANS Uterus • Layers: • serosa • muscular (myometrium) • mucosa (endometrium)
• The serosal layer is formed by the peritoneum that covers the uterus
INTERNAL GENERATIVE ORGANS Uterus: Myometrium • Bundles of smooth muscle united by connective tissue in which there are many elastic fibers • Relative more muscle in the inner wall than the outer wall, and in the anterior and posterior walls than in the lateral walls • Muscle fibers diminish caudally such that the muscle comprises only 10% of the tissue mass in the cervix • The interlacing myometrial fibers that surround the myometrial vessels are integral to control of bleeding from the placental site during the third stage of labor
INTERNAL GENERATIVE ORGANS Uterus: Endometrium thin, pink, velvet-like membrane perforated by a large number of minute ostia of the uterine glands. Histology Epithelium - single layer of closely packed high columnar cells than rests on a thin basement membrane Uterine glands – invaginations of the epithelieum that extend to the myometrium Interglandular mesenchymal stroma – varies remarkably throughout the ovarian cycle, undergoes decidualization following ovulation
INTERNAL GENERATIVE ORGANS Uterus: Blood supply
INTERNAL GENERATIVE ORGANS Uterus: Endometrium Vascular architecture • Uterine and ovarian arteries arcuate arteries radial arteries spiral/coiled arteries and basal/straight arteries • Spiral arteries – midportion and superficial third of the endometrium, responsive to hormones • Basal arteries – basal layer, not responsive to hormones
INTERNAL GENERATIVE ORGANS ROUND LIGAMENTS Extend from the lateral portion of the uterus Arise below and anterior to the origin of the oviducts. Terminate in the upper portion of the labium majus. Sampson artery runs within this ligament. Corresponds embryologically to the gubernaculum testis of men Clinically significant when doing puerperal tubal sterilization
INTERNAL GENERATIVE ORGANS BROAD LIGAMENTS • Winglike structures from lateral margins to pelvic sidewall • Each consist of an anterior leaf and a posterior leaf • Drapes over structures extending from the cornu • Mesosalpinx, mesoteres, mesovarium, mesometrium • Suspensory ligament or infundibulopelvic ligament – from the fimbriated end of the fallopian tube to the pelvic wall, where ovarian vessels traverse
INTERNAL GENERATIVE ORGANS CARDINAL LIGAMENTS Transverse cervical or Mackendrodt ligament Thick base of the broad ligament that is continuous with the connective tissue of the pelvic floor
INTERNAL GENERATIVE ORGANS UTEROSACRAL LIGAMENTS • From its attachment posterolaterally to the supravaginal portion of the cervix and inserts into the fascia over the sacram • Form the lateral boundaries of the pouch of Douglas
INTERNAL GENERATIVE ORGANS LYMPHATICS • Cervix • terminate mainly in the hypogastric nodes, which are situated near the bifurcation of the common iliac vessels.
• Body of the uterus • internal iliac nodes and periaortic lymph nodes
Blood Vessels
INTERNAL GENERATIVE ORGANS FALLOPIAN TUBES Also called oviducts Vary in length from 8 to 14 cm. lumen is lined by mucous membrane. PARTS interstitial portion isthmus ampulla infundibulum or fimbriated extremity- funnel-shaped opening at the distal
INTERNAL GENERATIVE ORGANS FALLOPIAN TUBES •
•
•
Tubal smooth muscle: inner circular and outer longitudinal, undergo rhythmic contraction or peristalsis toward the uterine cavity Epithelium in close with muscle layer because there is no submucosa Epithelium - columnar cells (some ciliated, others secretory)
INTERNAL GENERATIVE ORGANS Ovaries the ovaries vary considerably in size. During childbearing years, they are from 2.5 to 5 cm in length, 1.5 to 3 cm in breadth, and 0.6 to 1.5 cm in thickness. After menopause, ovarian size diminishes remarkably.
Rest in a slight depression on the lateral wall of the pelvis, called ovarian fossa of Waldeyer between the divergent external and internal iliac vessels Attached to the broad ligament by the mesovarium.
INTERNAL GENERATIVE ORGANS Ovaries PARTS: • Cortex- outer layer, contains oocytes and developing follicles • Medulla- central portion, composed of loose connective tissue BLOOD SUPPLY • The ovaries are supplied with both sympathetic nerves from the ovarian plexus and parasympathetic nerves.
THANK YOU!
Quiz
12 13
14,15 – Blood supply to the uterus
Quiz